Surgical therapy options
for pancreatic diseases
Operations on the pancreas are performed for a variety of reasons. The choice of method depends on the disease and the symptoms it causes. The surgeon discusses the planned operation with the patient before the operation. Occasionally, a slightly different picture emerges during the operation than discussed in the preliminary consultation, which requires a modified procedure. This possibility is also discussed before the operation.
Normal position of the pancreas
Page content
1. Surgical draining
This procedure will eliminate blocked pancreatic secretions caused by the disease. Most often the surgeon will operate on pseudo-cysts, found to have formed during pancreatitis. The surgeon will open up the cyst and connect it to an inactive loop of the small intestine. With this procedure, blocked secretions can be drained.
The entire pancreas may be opened, if the pancreatic duct becomes enlarged during chronic pancreatitis. The opened gland will then be sewn onto an inactive loop of the small intestine. This procedure will relieve pain, but can only temporarily correct misdirected secretion flows.
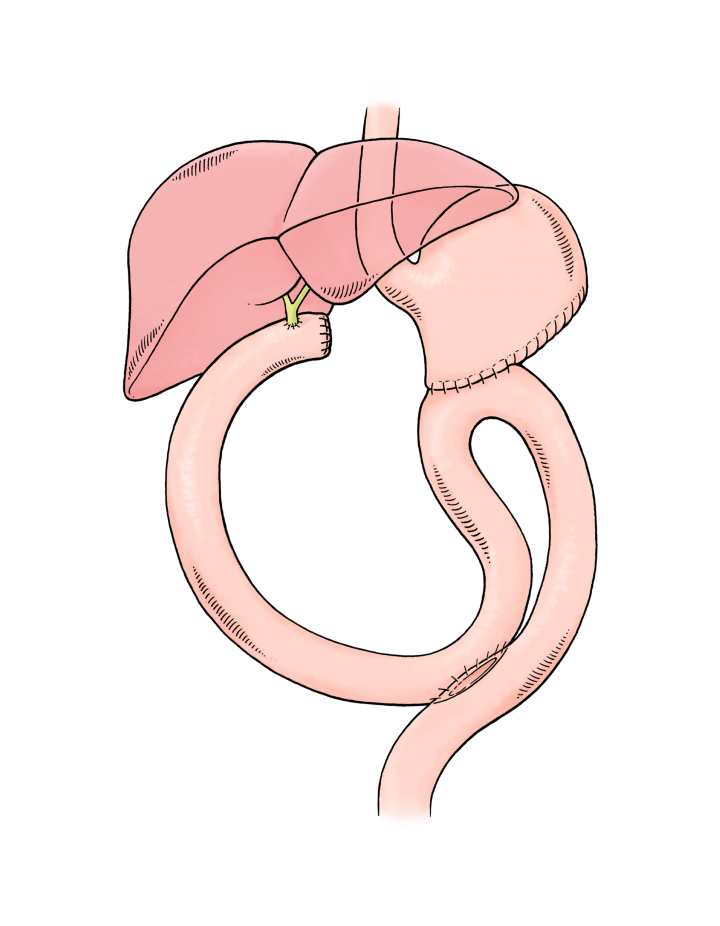
Food can no longer be passed on, if a tumour in the pancreas head blocks the duodenum. If the tumour cannot be removed totally, doctors will at least relieve pain and restore the patient's ability to eat normally. This procedure connects the stomach with the upper part of the small intestine, thus restoring food passage by bypassing the blocked duodenum, and it is known as gastroenterostomy.
Icterus (jaundice) will be found, if a tumour in the pancreas head prevents the flow of bile. Digestive malfunction and intense itching are often the consequences of the condition and joining the gall duct to the small intestine can bring relief. The procedure is known as biliodigestive anastomosis.
1. Surgical draining
2. Resection surgeries
Doctors must consider a variety of surgical procedures when dealing with pancreatic tumours or inflammation. Surgical and post-operative therapies are not always straightforward and will be tailor-made to the needs of the patient. One will always strive to preserve as much healthy tissue as possible. Maintaining a safe distance to the tumour when dealing with healthy tissue is crucial. Pathologists will determine that distance when they assess the affected tissue.
2.1 Left-sided pancreatic resection
The surgeon will choose this procedure if tail or body of the pancreas is cancerous or inflamed. A part - variable as to size -of the gland is removed. Usually, the pancreatic duct is closed at the separation line, and in a considerable number of cases, surgeons will connect the pancreatic duct to an inactive loop of the small intestine. Every attempt will be made to leave the spleen intact, but this will sometimes be impossible, as blood supply of pancreas tail and spleen often are connected. The surgeon will usually prevent later complications be removing the gall bladder as well.
Post-surgical condition of the patient will depend on how much of the pancreas remains. In many cases, digestive malfunctioning or diabetes mellitus can be avoided. A more pronounced tendency to thrombosis, due to a higher number of thrombocytes, can emerge if the spleen was removed, as the body's patterns to fight infection will change.
2.1 Left-sided pancreatic resection
2.2 Duodenum-preserving pancreatic head resection
This procedure will assist with the therapy of chronic pancreatitis. It will limit the loss of healthy tissue and therefore protect organs more effectively. Long-term damage is avoided while results are similar or better when compared to procedures used in the past.
The surgeon will sever connections between the pancreas head and the duodenum, a technically very difficult procedure. The bile duct must be left untouched to avoid any disruption of bile flow into the duodenum. The remainder of the pancreas is then sewn onto an inactive loop of the small intestine. This component of the procedure is particularly demanding, as aggressive pancreas secretions constantly affect the joined sections of pancreas, pancreatic duct and sewn-on small intestine.
The gall bladder is removed to prevent later complications with the flow of bile. Stomach and duodenum are not affected in the procedure. Remaining pancreatic secretions are merged in the upper section of the small intestines with food and bile. This ensures that the patient's digestive system will perform normally. It is sometimes necessary to sew the bile duct onto a loop of the small intestine. This will be done if the bile duct cannot be separated from inflamed pancreatic tissue (this is known as biliodigestive anastomosis). Success again depends on the degree to which pancreatic function has been reduced or lost. With lessening pain the patient will usually be able to eat normally. If this can be achieved, the doctor will be able to assess the patient's metabolism as to robustness and decide on an effective therapy (enzyme substitution, diabetic therapy, vitamin supplements).
2.2 Duodenum-preserving pancreatic head resection
2.3 Pancreas Head Resection (Kausch/Whipple procedure)
This procedure has been performed since the beginning of last century. From the 1950s, with improved anaesthetic technology as a backdrop, the procedure became the standard therapy for cancer of the pancreas head. Today, we still use the same method, however a host of variations has evolved in the meantime. The classic Whipple method involves the removal of 2/3 of the stomach, gall bladder, pancreas head and duodenum. Thus the surgeon can access the important lymph vessels, known as lymph nodes. For safety reasons these must be removed and assessed by the pathologist. It is here that the first small metastases, escapees of the pancreatic tumour will be found.
It is difficult to connect the remainder of the pancreas to a non-active loop of the small intestine, because aggressive pancreatic secretions will affect seams produced during the anastomosis between intestine, pancreatic duct and pancreas tissue. The bile ducts needs to be sewn onto a deactivated loop of the small intestine as well, since the duodenum has been removed.
These days, surgeons often use a variation of the Whipple procedure to preserve the stomach. Doctors refer to this procedure as the pylorus-preserving pancreas head resection according to Traverso (pylorus is the stomach gateway).
Diverse conditions can give rise to unwanted post-operatic fallout, when this proce- dure is applied. Loss of pancreatic functions with associated symptoms (lack of enzymes, diabetes mellitus and lack of vitamin absorption) depends on how much pancreatic tissue has been removed. Complications may also emerge, if the stomach was partly removed (dumping syndrome, lack of vitamin B12, incompatible bacteria in the small intestines etc).
Constriction of gall duct anastomosis with ensuing obstruction of gall flows or, as pointed out above, incompatible bacteria in the small intestines can lead to ascending inflammation of the gall duct. A narrowing of the anastomosis can lead to an obstruction in the food passage through the stomach outlet when using the abovementioned organ-preserving procedure.
2.3.1 Pancreas Head Resection (Kausch/Whipple procedure)
2.3.2 Pylorus-preserving pancreas head resection according to Traverso
2.4 Pancreatic head preserving duodenal resection
This recently developed procedure allows the surgeon to preserve the pancreas head when cancer is found in the papil (combined gall and pancreas secretion duct), by removing only the duodenum. Complicated sewing techniques must be used, as pancreas duct, bile duct and stomach must be attached to the small intestine, however the surgeon will be able to preserve the organs. The Whipple procedure would have previously been unavoidable in this case.
Negative results can only arise through faulty anastomosis. No long-term statistical results are yet available for this recently developed procedure.
2.4 Pancreatic head preserving duodenal resection
2.5 Total Pancreatectomy
This procedure involves disposing of the entire gland. 2/3 of spleen, stomach, duodenum and gall bladder are removed along with the pancreas. Technically speaking, pancreatectomy is easier to perform than the classic Whipple procedure, as no anastomosis needs to be applied. As with other procedures, the smaller-size stomach needs to be connected with the small intestine. However unwanted out- comes can be considerably more serious. The operation is therefore only used as a last resort, when it is not possible to preserve pancreatic tissue by any means. In any case, the bile duct must be connected to an inactive loop of the small intestine. Many variants of the procedure exist these days, e.g. surgeons will attempt to preserve stomach and/or spleen.
The main issue with this procedure is the patient's metabolism. This type of diabetes is difficult to control as both insulin and its counterpart, glucagon are no longer produced. As a result the patient is exposed to a high risk of hypoglycaemia (lack of blood sugar). Similar unwanted complications (cf. Whipple procedure) can also emerge here, but they are of a more serious nature, as diabetes sufferers must keep up a constant intake of food to avoid a drop in blood sugar levels.
Removal of the spleen weakens the patient's infection resistance and often causes a substantial increase in the number of thrombocytes (blood platelets). Thus, an elevated risk of thrombosis is unavoidable (that risk is at any rate considerable in cancer patients).
2.5 Total Pancreatectomy
2.6 Segmental resection of the pancreas
Sometimes it is possible to remove a small tumour in the body of the pancreas without damaging or removing other organs. Thus, a pancreas head with duodenum and a pancreas tail with spleen can be preserved. To connect the remaining parts of the pancreas with the intestines can be difficult in this procedure. Either the pancreas head is sealed at the end and pancreatic fluid (insulin) will then flow into the duodenum, or the surgeon will connect a loop of the small intestine with pancreatic duct and tissue. This loop must also collect pancreatic secretions emanating from the pancreas tail. Insulin or pancreatic enzyme deficiencies are usually not the cause of a negative outcome. It is more likely that the degree of technical difficulty encountered in this procedure will generate problems. Hence, the operation should only be performed in specialised clinics.